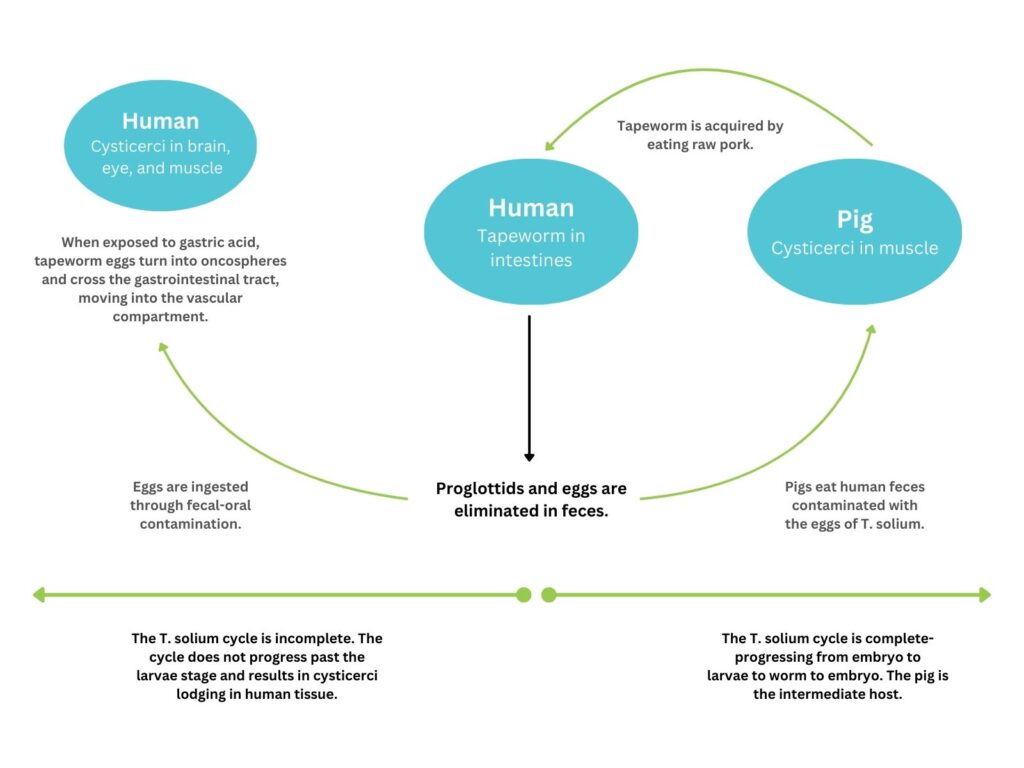
Neurocysticercosis is a parasitic infection resulting from ingesting eggs from the adult tapeworm, Taenia solium. This central nervous system manifestation of cysticercosis is the most common parasitic brain infection and a leading cause of epilepsy in the developing world.
- In recent years, neurocysticercosis has become a significant cause of seizures, accounting for up to 10% of emergency room visits for seizures.
Natural History
- Acquired through consuming contaminated food with the feces of a T. solium tapeworm carrier (fecal-oral contact).
- Tapeworm eggs, shed in stool, contaminate food through poor hygiene.
- Ingested eggs transform into larval cysts (oncospheres) in the human stomach.
- Oncospheres migrate to the brain, muscles, eyes, and other structures via the vascular system.
- Larval cysts may remain viable in the brain for years.
Epidemiology
- Endemic in Central and South America, Asia, and Africa.
- Linked to poor sanitation and hygiene.
- No gender or race predilection; affects symptomatic patients aged 15-40 years.
Clinical Presentation
- Seizures: Most common symptom, a leading cause of seizures in young adults in endemic areas.
- Headaches
- Hydrocephalus
- Altered mental status
- Neurological deficits
Stages of Neurocysticercosis
- Vesicular: Viable parasite with intact membrane; no host reaction.
- Colloidal Vesicular: Parasite dies within 4-5 years, cyst fluid becomes turbid; most symptomatic stage.
- Granular Nodular: Edema decreases, cyst retracts, enhancing persists.
- Nodular Calcified: End-stage quiescent calcified cyst remnant; no edema.
Location
- Cysts can occur intraaxially or extraaxially in the neuraxis.
- Parenchyma: Most common, usually involving the grey-white matter junction.
- Subarachnoid space over the cerebral hemispheres: Can be very large.
- Ventricles
- Spinal forms: Usually associated with concomitant intracranial involvement.
Imaging Features by Stage
- Vesicular Stage
- Cyst with dot sign.
- CSF density/intensity.
- Eccentric hyperintense scolex on T1.
- No enhancement; no surrounding vasogenic edema.
- Colloidal Vesicular Stage
- Turbid cyst fluid.
- CT: Hyperattenuating to CSF.
- MRI T1: Hyperintense to CSF.
- Surrounding edema; thickened, brightly enhancing cyst wall.
- Granular Nodular Stage
- Edema decreases.
- Cyst retracts, becoming a small enhancing nodule.
- Less marked enhancement persists.
- Nodular Calcified Stage
- Quiescent calcified nodule.
- No edema.
- No enhancement on CT.
- Signal drop-out on T2 and T2* sequences.
- Long-term enhancement may predict ongoing seizures.
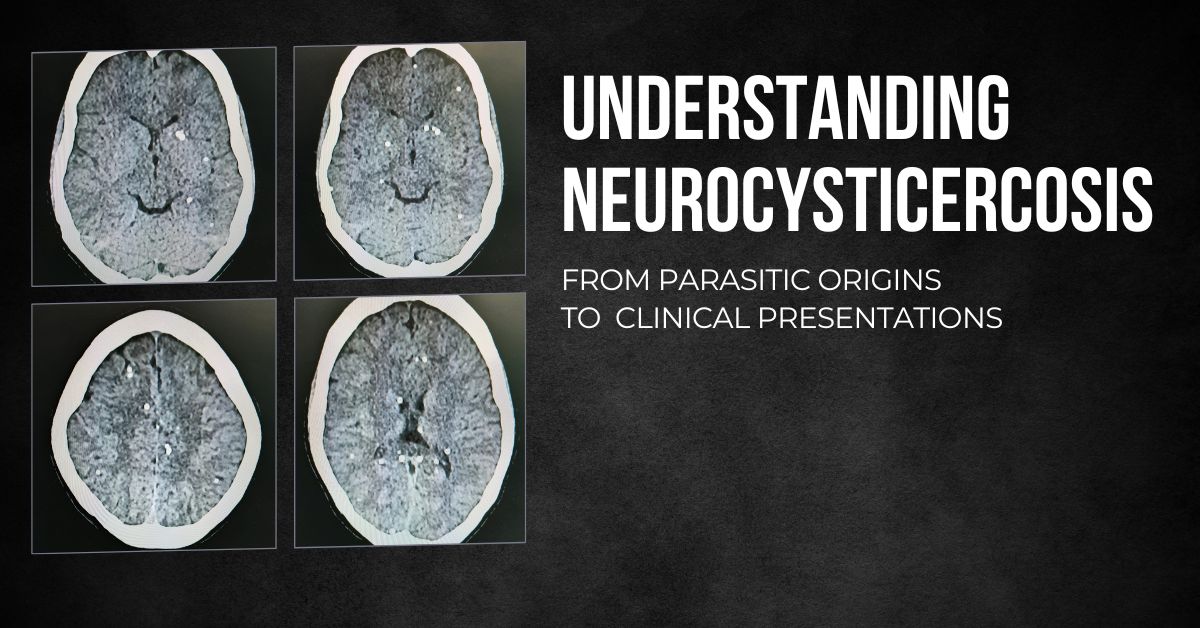
Case Report
- Patient:
- Age: 34-year-old male.
- Clinical Presentation: Headache & Seizure.
- NCCT Brain Findings:
- Multiple calcified 3-7 mm nodules scattered throughout the bilateral cerebral hemispheres.
- Some nodules causing minimal surrounding edema, particularly in the left frontal lobe.
- Indicative of varying stages of healed neurocysticercosis.